Safety 1st Deluxe 25-Piece Baby Healthcare and Grooming Kit (Arctic Blue)
$21.04 (as of April 8, 2024 16:21 GMT +00:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)Compact and convenient, this deluxe healthcare kit makes a great baby shower gift. It is small enough to carry in a diaper bag or in a stroller for visits to the park or when traveling. The grooming kit portion includes a newborn cradle cap comb, a G... read more
Latest Blog Posts
How to Sleep After Gallbladder Surgery: Comprehensive Guide
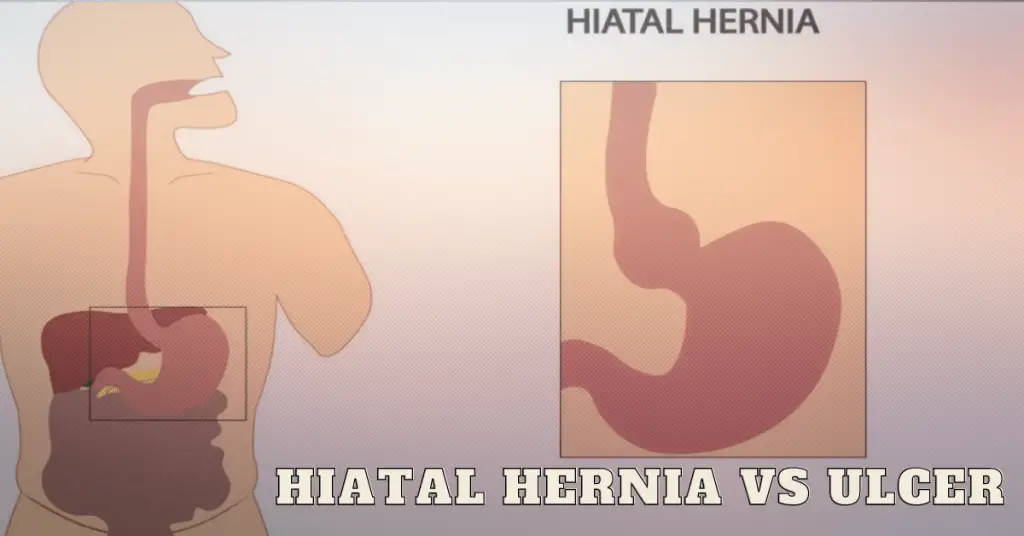
Demystifying Hiatal Hernia vs Ulcer: Understanding the Differences
Why is My Stomach Bigger After Gallbladder Surgery?
Gastritis vs. Gallbladder: Understanding the Differences, Symptoms, and Treatment Options
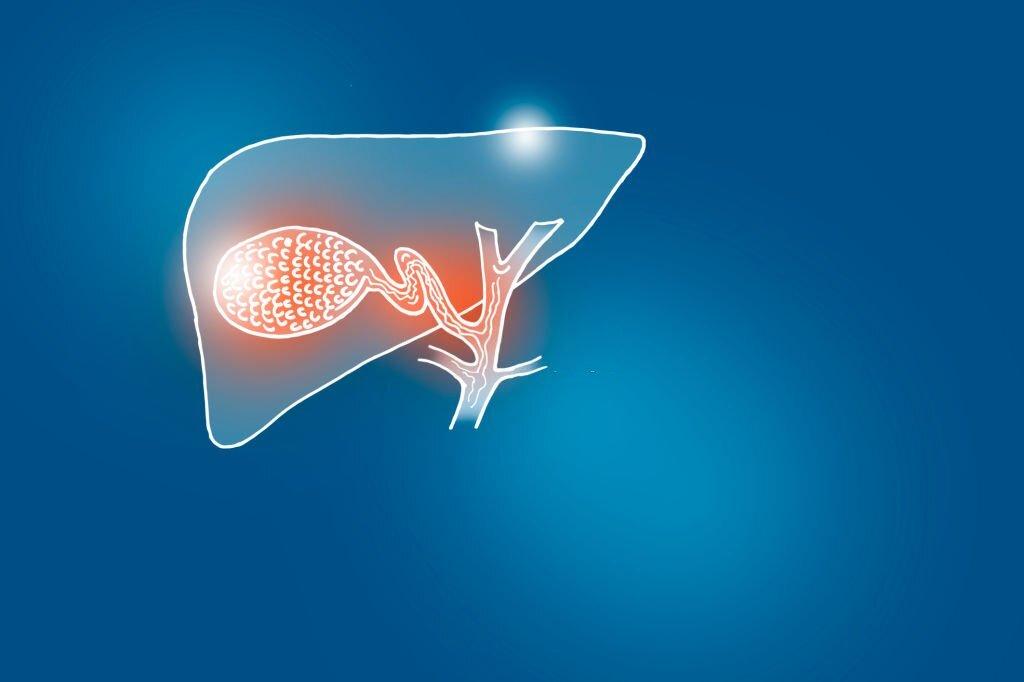
Unveiling the Phrygian Cap of the Gallbladder: prognosis, Surgical Considerations, complications, and Research Insights
Can a Gallbladder Grow Back Afer Surgery
Bile Reflux And Acid Reflux After Gallbladder Surgery | Cholecystectomy
The Spiritual Meaning Of Gallbladder
How Much Does A Gallbladder Weigh
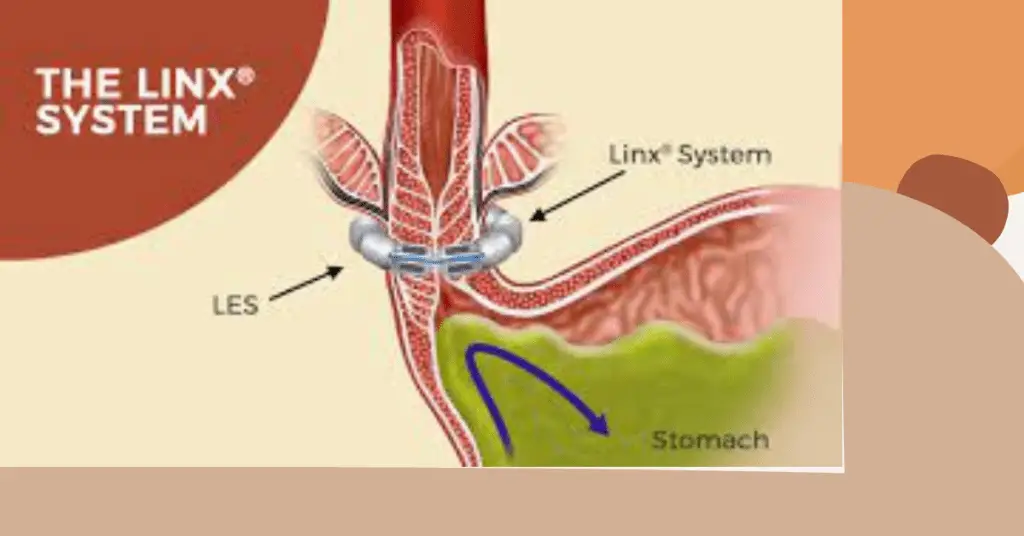
Pros and Cons of the LINX Surgery
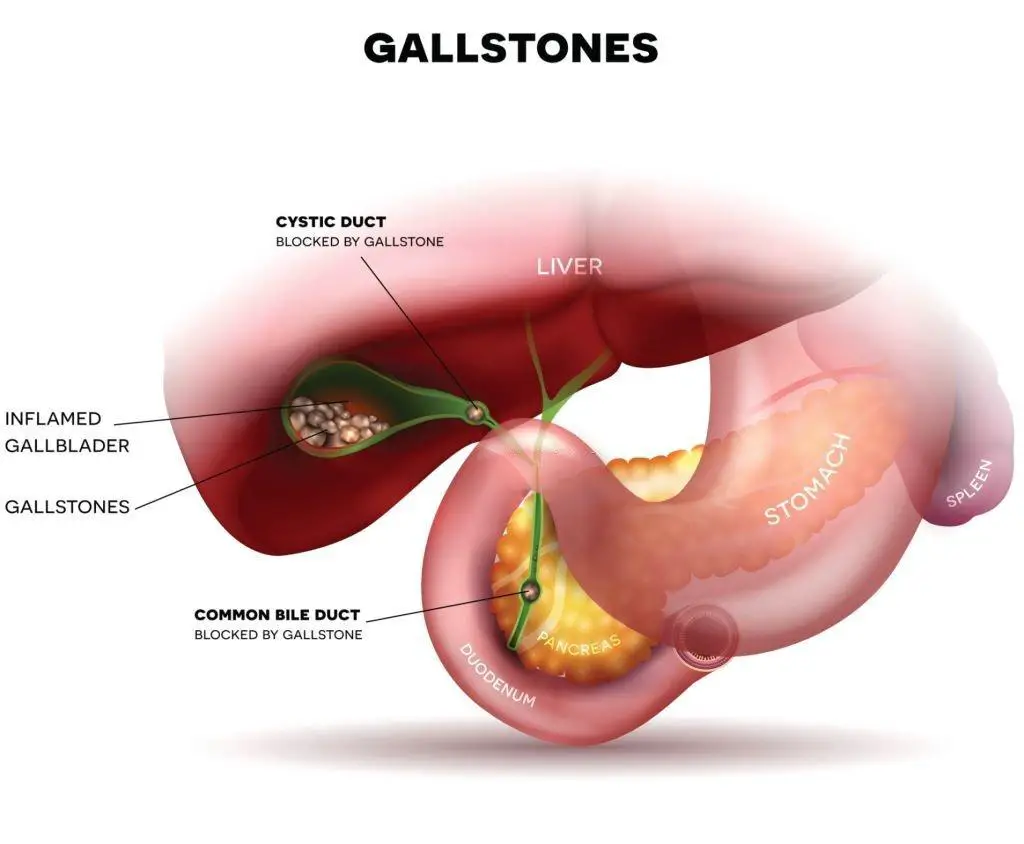
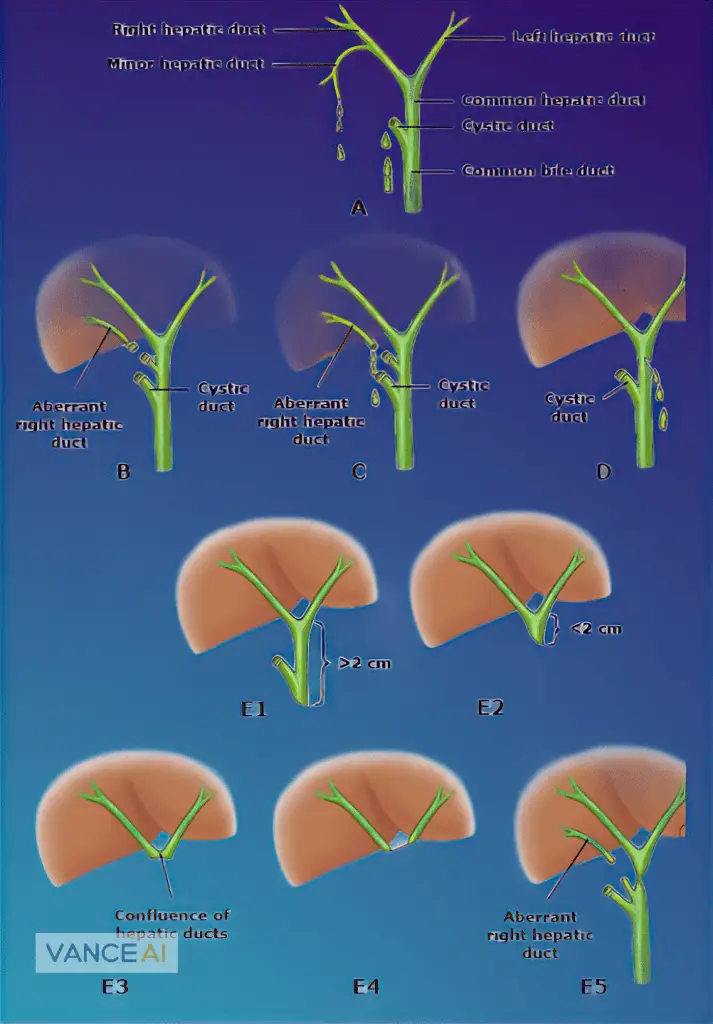
Bile Duct Injuries During Gallbladder Surgery
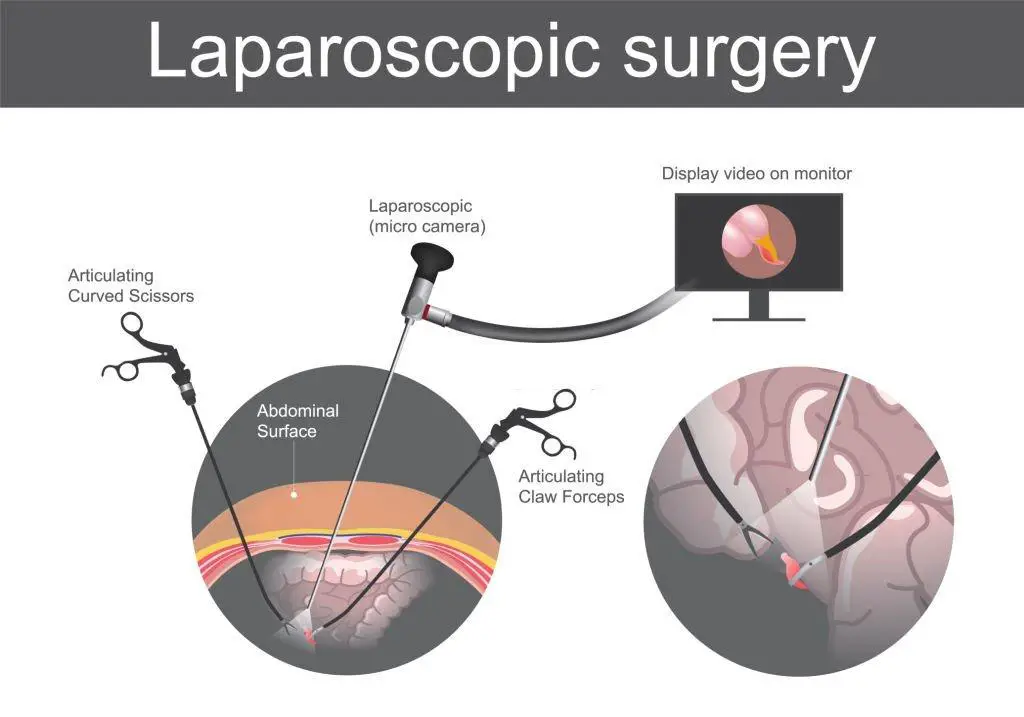
Laparoscopic Cholecystectomy | GallBladder Surgery: A Comprehensive Guide
Baby Sound Machine, Momcozy White Noise Machine for Baby Sleeping with Night Light, Toddler Sleep Trainer with 34 Soothing Sounds, Timer, App Remote Control, Personal Sleep Routine (Blue)
$39.99 ($2.64 / Ounce) (as of April 8, 2024 16:21 GMT +00:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)【Multiple Soothing Sounds】34 high-fidelity sounds (11 white noises, 3 fan sounds,8 lullabies and 12 nature sounds) ,40~110dB, let you choose the ideal background to mask intruding noises and create the perfect environment for work, study, sleep or an... read more